What does it take to fight the world’s number one killer?
A silent pandemic is sweeping across the world: Non-communicable diseases. In Bangladesh, over 70% of deaths can now be attributed to diseases like hypertension and diabetes. A new initiative by the Government of Bangladesh, BRAC and Medtronic Labs is showing promising results in changing that.

BY Simin Ibnat Dharitree and Dr Imran Ahmed Chowdhury
This piece was originally published on The Good Feed. It has been republished here.
Ashamoni’s front yard consists of piles of bricks, mounds of sand, and bags of cement. All the ingredients to build a house, but suddenly no money to do it. Everything had been going fine until three weeks ago, when Ashamoni’s father died suddenly of a stroke, aged just 40. It was a painful shock. It was not isolated, though — Ashamoni’s uncle died from a similar sudden stroke two years earlier. Both her father and uncle suffered from hypertension. Their deaths are part of a silent pandemic sweeping across the world, which is particularly pronounced in Bangladesh, where over 70% of deaths can now be attributed to diseases like hypertension and diabetes. And this is just the tip of the iceberg — it is estimated in Bangladesh that half of these diseases are still undiagnosed. A new initiative by the Government of Bangladesh, BRAC and Medtronic Labs is showing promising results in changing that.
It has been over 75 years now since treatments for diabetes and hypertension were discovered — yet these diseases continue to be the world’s number one killer.
Deaths caused by non-communicable diseases (NCDs) now account for 75% of deaths globally. It is even higher in low and middle-income countries, where these diseases can now be linked to almost 80% of deaths globally.
Non-communicable diseases also have massive ripple effects — because of their effects on quality of life, but also because of the prohibitive costs associated with them. People with non-communicable diseases like hypertension and diabetes generally require medication for life, and are often hospitalized multiple times during their lifetimes. Bangladesh has the second highest out of pocket expenditure in the world, behind only Afghanistan, so these costs end up being borne mostly by individuals. This has clear broader societal impacts — each year health expenses drive 6.1 million people in Bangladesh into poverty. Anecdotal evidence from BRAC’s staff on the ground suggests this is particularly prevalent in urban slums, where households are now spending up to half of their income on medical bills.
A new collaboration that’s starting to turn the tide
In Bangladesh, a new initiative by the Government of Bangladesh, BRAC and Medtronic, a global leader in healthcare technology, is showing promising results in turning this tide. Piloted so far in two districts in the country, the initiative — titled NCD360° — has managed to almost triple the control rates of hypertension, bringing them up from 31% to 78%, and almost double the control rates of diabetes, bringing them up from 23% to 41%.
 A paramedic checking the blood pressure of his patient in a community clinic in northern Bangladesh. © BRAC
A paramedic checking the blood pressure of his patient in a community clinic in northern Bangladesh. © BRAC
NCD360° builds on a decade of efforts by the Government of Bangladesh. By the turn of the 21st century, the non-communicable disease epidemic in Bangladesh was becoming too big to go unnoticed. In 2012, the government redeveloped the public healthcare policy and started opening dedicated non-communicable disease corners in upazila health complexes — frontline public hospitals in each subdistrict. The corners were designed to have a dedicated doctor and nurse who would diagnose and consult patients and provide free medicine. Bangladesh now has more than 400 such corners across the country.
The corners made some impact, but large-scale progress was hindered by a combination of factors — a lack of doctors and nurses willing to work in them, insufficient budget for the quantity of medicine needed, but — most critically — a lack of public awareness about non-communicable diseases.
While these diseases are critical, they are also slow-onset, so create a false sense of security.
In 2023, the government partnered with BRAC and Medtronic to figure out how to raise health-seeking behavior. The resulting initiative — NCD360° — draws on BRAC’s extensive network of community health workers, and a customized technology solution from Medtronic. NCD360° was implemented in the two districts of Bangladesh with the highest rates of non-communicable diseases — Nilphamari, in northwestern Bangladesh, and Narayanganj in central Bangladesh.
Taking awareness — and technology — to doorsteps
NCD360° saw hundreds of BRAC community health workers add awareness raising, screening and follow-ups for non-communicable diseases to their regular door-to-door visits. During each visit, they use a mobile app to submit blood sugar and blood pressure levels. The app tells them whether there is a concern, and the person should be referred to a frontline government primary health outpost, or community health clinic — or whether the patient has a critical condition and needs to be referred directly to an NCD corner.
If the person is referred to a community clinic, a government health care provider does a basic assessment and refers them to the nearby NCD corner. If the person is referred to an NCD corner, a nurse diagnoses the person’s condition, and a doctor then diagnoses the person’s condition and prescribes treatment, and then a health educator from BRAC sits with the person to explain the treatment and counsel on necessary lifestyle modification requirements, self care — and answers any questions they may have. Community health workers, supported by staff in a dedicated call center, then follow up regularly until the patient’s disease is under control.
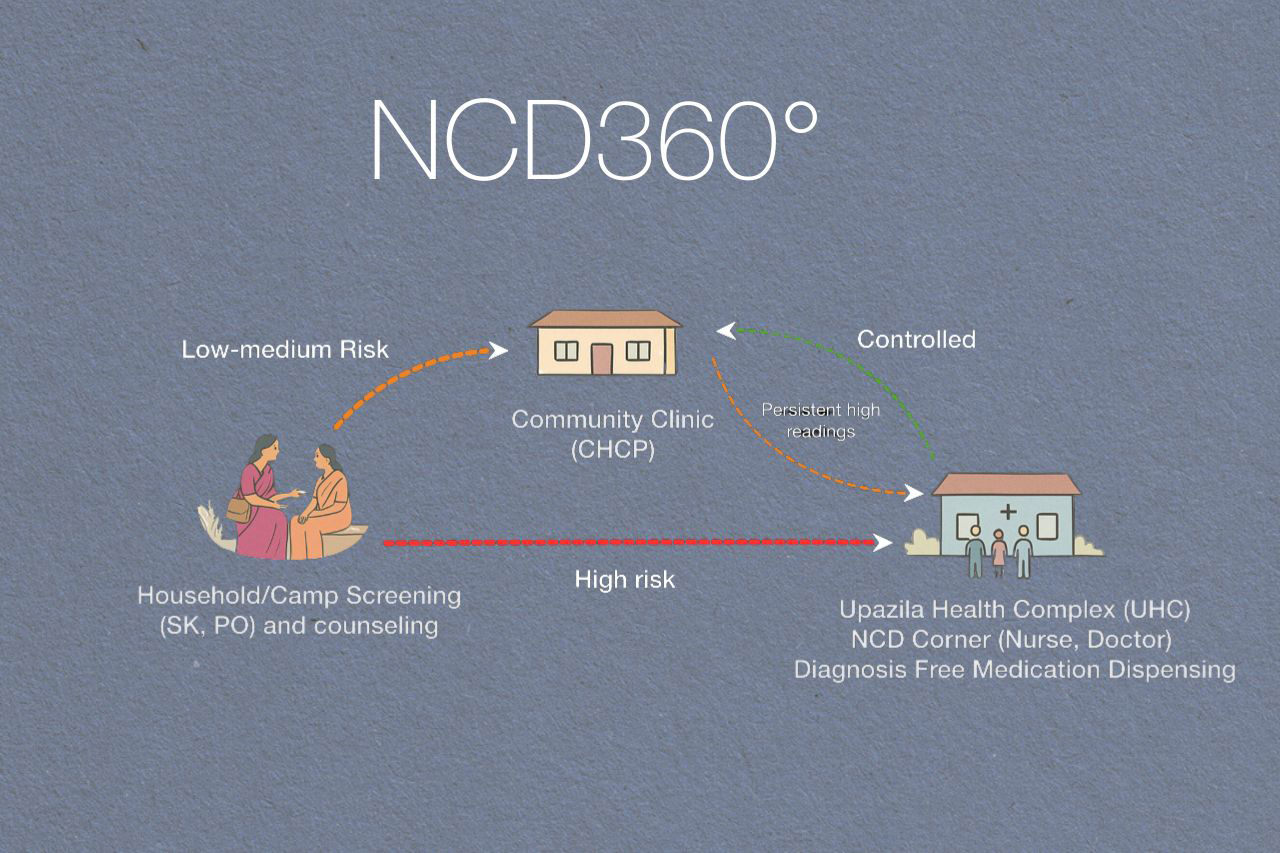 This is how NCD360° functions on the ground. © BRAC
This is how NCD360° functions on the ground. © BRAC
NCD360° initiative has screened one-third of the people who are over 40 years old in the five subdistricts of these two districts over the last two years, amounting to 169,274 people. Health-seeking behavior has noticeably risen — almost a quarter of the people that were referred to and received healthcare in NCD corners during this period were referred by community health workers. The initiative has also sparked a broader ripple effect. General awareness about non-communicable diseases is growing, and increased traffic into NCD corners is fostering a heightened sense of accountability among doctors and nurses in them, which is also supporting the flow of medicines to the corners. The initiative has been likened to adding an electrical connection between the community and the existing government health infrastructures, sparking a current that is enlivening the whole system.
The initiative is now being scaled to five more districts in northern Bangladesh where the burden of non-communicable diseases are particularly high. A lot is still to be figured out, though. As an example, only 1 in 3 people referred for diagnosis actually enrolled in the system and went on to receive care. Similarly, a large number of people, like Ashamoni’s father and uncle, get diagnosed but then do not follow the treatment.
 The whole system is tied together with a mobile app which connects community health workers, community clinics, NCD Corner with the central control room in the capital. © BRAC
The whole system is tied together with a mobile app which connects community health workers, community clinics, NCD Corner with the central control room in the capital. © BRAC
The potential goes beyond non-communicable diseases — and beyond Bangladesh
Just as non-communicable diseases have ripple effects on other conditions in a person’s body, a lack of investment in non-communicable diseases has ripple effects across societies.
Non-communicable diseases will be the leading cause of disability across the world by 2030. In Bangladesh, non-communicable diseases are already the cause of 63% of disabilities. Investments in holistic public health solutions offer up to seven-fold returns, by reducing premature deaths, illness and disability.
Health shocks are also a clear cause of poverty, and there are broader societal concerns as well, such as children like Ashamoni being at higher risk of child marriage as a result of her father’s death.
With deaths linked to non-communicable diseases projected to increase by 17% in the next decade, and health budgets shrinking globally, we need to be thinking differently about how we can tackle this wave. One way is by combining the strengths of community-based non-governmental organizations, advancements in technology, and leveraging public investments.
NCD 360° is a decentralized model bringing care to the communities’ homes. The 360° approach is a digitally supported community-based holistic intervention, significantly improving disease detection and clinical outcomes. Community-based strategies can effectively manage diabetes, hypertension, and other chronic conditions. This model works by equipping community health workers with technology for better decision making and creating connected care networks. Bangladesh is showing promising health outcomes while maintaining accessible and affordable care at the community level. This is a value-based primary healthcare model for NCDs that can be scaled in Bangladesh and could be adapted in different country contexts. The NCD 360° model was piloted in five sub-districts in Narayanganj and Nilphamari. It has been scaled up in 37 subdistricts of 7 districts of Bangladesh.
Simin Ibnat Dharitree is a Communications Consultant at BRAC. Dr. Imran Ahmed Chowdhury is the Program Head of BRAC’s health program.